Seed Grant 2022 Recipients
Meet our 2022 Seed Grant recipients! Each of these leading laboratories will receive no-cost access to the available inventory of Amnion Foundation cells and reagents to support high-impact projects in drug development, toxicology, and regenerative medicine.
Dr. Pouria Fattahi – University Of Pennsylvania
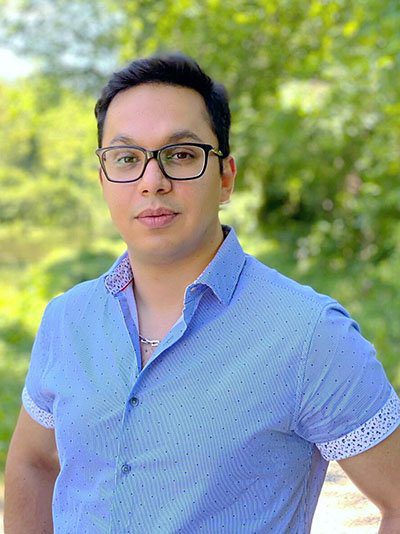
Dr. Pouria Fattahi, a senior postdoctoral researcher in Dan Huh’s group in the Department of Bioengineering at the University of Pennsylvania, has been selected as the recipient of the Amnion Foundation Seed Grant (AFSG) award to develop a human placenta-on-a-chip, a novel microengineered in vitro model of the maternal-fetal interface in the human placenta. Dr. Fattahi aims to harness the power of this biologically inspired innovative microtechnology to discover and mechanistically investigate the adverse effects of heavy materials on human pregnancy, which represents a long-standing challenge in reproductive science.
Exposure of pregnant women to heavy metals is a major public health concern around the world. Over the last decades, a mounting body of evidence has shown the deleterious potential of sustained heavy metal exposures to cause various types of pregnancy complications that can be detrimental to fetal development. Despite the increasing prevalence and significance of this problem, however, it remains a major challenge to understand and predict reproductive toxicity of heavy metals due to the ethical, scientific, and practical issues associated with human pregnancy research. Motivated by this critical challenge, a team led by Dr. Fattahi is partnering with environmental toxicologists and clinicians in reproductive medicine to create a bioengineered analog of the human placenta and use this biomimetic system as a novel platform for preclinical study of heavy metal toxicity in human pregnancy. Specifically, the team is developing a unique approach where human trophoblast cells and fetal endothelial cells are grown together in a microfabricated device the size of a memory stick to replicate the structure and function of the placental barrier between maternal and fetal blood. Using these lab-grown human placental tissues in a microchip, the research team is attempting to tackle the long-standing question of whether and how heavy metals such as cadmium present in the maternal circulation can transfer to or be excluded from the blood of developing fetus.
Dr. Fattahi plans to use the funds provided by the AFSG award to obtain primary human placental cells including cytotrophoblasts, microvascular endothelial cells, and Hofbauer cells to construct a more advanced, realistic placenta-on-a-chip model to accelerate the progress of his ongoing work. Dr. Fattahi believes that this new effort enabled by the AFSG grant will make great contributions to realizing his exciting vision of pioneering innovative bioengineering technologies towards the ultimate goal of advancing our understanding of how environmental exposures can change the course of the most fundamental process of life.
BIOLines Laboratory: https://biolines.seas.upenn.edu/index.html

Alex Goudreau – University Of Ottawa, Canada

Alex Goudreau, a Master’s candidate in Dr. Kristi Adamo’s lab at the University of Ottawa has received a Seed Grant from the Amnion Foundation to support a project examining the impacts of physical activity during pregnancy. As Dr. George R Saade said, “There is nothing in medicine that can return so much on an investment as a healthy pregnancy and delivery, because that has years and years of impact later. And placental health is critical to the health of a pregnancy.” The placenta is a temporary organ which provides the fetus with oxygen and nutrients during pregnancy. Physical activity (PA) during pregnancy supports a healthy mom, baby, and placenta. How these benefits arise is yet to be fully understood. In the non-pregnant population, regular PA leads to changes in the immune system to an anti-inflammatory profile. Placenta-resident immune cells, known as Hofbauer cells, reflect the ability of other macrophage subtypes to polarize between pro- and anti-inflammatory states. While Hofbauer cells exist in a predominantly anti-inflammatory state, changes in polarization state have been associated with adverse health outcomes such as pre-eclampsia, gestational diabetes, and pre-term birth. The purpose of this novel study is to explore how substitutes for physical activity affect the polarization and gene expression of Hofbauer cells. It is necessary to fully understand these mechanisms before effective clinical strategies can be developed to protect against pregnancy complications and downstream/future health effects.
The Adamo Lab: http://www.adamolab.com/

Victoria Karakis – NC State University
Victoria Karakis, a doctoral candidate in the Balaji Rao Laboratory at NC State University has received a Seed Grant from the Amnion Foundation to support a project delving into the generation of trophoblast stem cells from term cytotrophoblasts. Many pregnancy-related pathologies have their origins in abnormalities arising during early placental development. Yet, there exists a critical knowledge gap in our understanding of early human placental development due to restrictions on research with human embryos and their limited availability. Moreover, there are significant differences between placental development in humans and commonly used animal models. In this context, human trophoblast stem cells (hTSCs), first derived from blastocyst-stage embryos and first trimester placentas by Okae et al. in 2018, have gained prominence as a powerful in vitro model for studies on early placental development. Similar to the epithelial cytotrophoblast (CTB) in the first trimester of gestation, hTSCs can differentiate to form extravillous trophoblasts (EVTs) and the multinucleate syncytiotrophoblast (STB). Here we propose to derive hTSCs by reprogramming of CTBs from term placentas in cell culture, without any genetic manipulation. Notably, the widely used conditions described by Okae et al. do not support culture of CTBs from term placentas. Our results will enable the use of term placentas as a source of cells to establish hTSC-based in vitro models of early human placental development.
Rao Research Group: https://www.cbe.ncsu.edu/raogroup/


Dr. Omar Perez, PhD, PharmD – University Of Illinois At Chicago, College Of Medicine

During pregnancy, the placenta acts as an interface between the fetus and the expecting mother. Moreover, the placenta functions as a barrier to protect the fetus against pathogens. Unfortunately, various pathogens, such as Zika virus (ZIKV), have found a way to bypass the placenta and infect the developing fetus. It remains unclear how ZIKV gains access to the fetal compartment and evades cellular antiviral pathways. Therefore, there is an urgent need to develop models to better understand the mechanism of mother-to-fetus transmission of ZIKV. In this present study, we propose to develop a novel co-culture system that better reflects the maternal-fetus interface. Hofbauer cells, cytotrophoblast cells and decidual immune cells will be co-cultured in a transwell culture system. This co culture system will allow us to:
1) Examine the role of decidual cells during ZIKV infection,
2) Explore the integrity of the tight junctions of the cytotrophoblasts during ZIKV infection,
3) Unravel the anti-viral intracellular innate response to ZIKV infection in the different cell types,
4) Understand the role of Hofbauer cells during ZIKV infection, and
5) Establish the mechanism of how ZIKV traverses the placenta to infect Hofbauer cells. Collectively, these data will provide a new model to study ZIKV infection and offer important insights into the mechanism of ZIKV transmission from mother-to-fetus.

Dr. Liliya Yamaleyeva, MD, MS – Wake Forest University, School Of Medicine

Dr. Liliya Yamaleyeva, Associate Professor in the Hypertension and Vascular Research Center at Wake Forest School of Medicine received a Seed Grant award to support the development of an in-vitro model of hypertensive disorders of pregnancy. Pregnancy related complications impact women’s health not only during pregnancy but also throughout her life. Hypertensive pregnancy disorders including preeclampsia complicate about 5-10% of all pregnancy cases, and represent one of the leading causes of maternal morbidity and mortality. The main focus of our research is on cardiovascular complications of pregnancy associated with placental disease. With the use of placental cells provided through the Amnion Foundation Seed Grant mechanism (trophoblasts, endothelial cells, and macrophages), we will be able to establish clinically relevant three-dimensional models of placental cell cultures to study the mechanisms driving the dysregulation of placental environment. These models will also provide a platform for our future research on the effects of various factors related to cardiovascular health on placental cell function as well as testing the possible therapeutic options for preeclampsia.
Liliya Yamaleyeva: https://school.wakehealth.edu/Faculty/Y/Liliya-M-Yamaleyeva
